
Existing methods of treating cervical osteochondrosis are aimed at reducing symptoms, preventing complications, stopping further destruction of the cartilage and bone tissue of the spine, and preventing the patient from becoming disabled.
Osteochondrosis is a pathological degenerative-destructive process that first captures the intervertebral disc, and then the vertebra itself.
It is necessary to treat osteochondrosis of the cervical region immediately after the first signs of the disease appear.
Mechanisms for the development of osteochondrosis.
The spinal column is made up of the vertebrae and the intervertebral discs located between them. The intervertebral disc has a gel-like nucleus pulposus in the center, surrounded on the periphery by a dense annulus fibrosus. The nucleus pulposus is hydrophilic, saturated with moisture and characterized by great elasticity. Due to the elastic properties of the intervertebral discs, cushioning and mobility of the spine are provided.
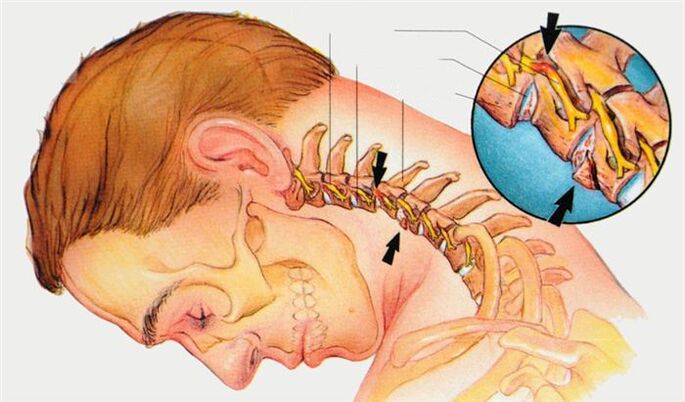
In people over the age of 20, the discs already begin to gradually lose their elasticity. This is due to the obliteration of the vessels that feed the discs, and the additional blood supply is due to diffusion from the bodies of the adjacent vertebrae. In cartilage tissue, against the background of a lack of nutrients, the regeneration processes slow down - the disc begins to "age". Initially, the nucleus pulposus dehydrates, loses its elasticity, flattens, which increases the load on the annulus fibrosus. Microcracks, stress zones, ruptures, delamination appear in the structure of the ring.
The degenerated disc bulges into the spinal canal and irritates the nerve endings of pain receptors located in the posterior longitudinal ligament.
The features of the pathological process in cervical osteochondrosis are associated with the anatomical structure of this spine: different structure and size of the cervical vertebrae, narrower articulation in the intervertebral joints, and underdeveloped muscular framework. With a prolonged static load on the cervical region (work at a computer), weak muscles do not hold the head well, and the main load falls on the spine.
Treatment of cervical osteochondrosis in a specialized clinic is carried out using a unique technology based on a combination of manual therapy, electrophoresis and photodynamic laser therapy under the supervision of doctors.
The main reasons leading to the development of osteochondrosis:
- Congenital or acquired abnormalities of the spine.
- Natural aging processes of the body.
- genetic predisposition.
- Long-term static and dynamic overload of the spine: forced posture, hypodynamia.
- Passion for dangerous sports for the spine: professional wrestling.
- Of smoking.
- Autoimmune diseases with connective tissue damage - collagenosis.
- Inadequate diet with a predominance of carbohydrates and fatty foods, with a deficiency of proteins, vitamins, micro and macro elements.
- Overweight, obesity.
- Spinal injuries and diseases.
Osteochondrosis of the spine: is there such a diagnosis?
In English medicine, this term refers to a completely different group of diseases that have nothing to do with our "native" osteochondrosis. In the International Classification of Diseases, a book that all neurologists should be guided by when indicating a diagnosis, there are terms such as "osteochondrosis of the spine in adults", "juvenile osteochondrosis of the spine", "osteochondrosis of the spine, unspecified ".
However, sometimes this diagnosis is not entirely justified, when the doctor cannot really fully understand what is happening to the patient. Under this term, diseases such as:
- myofascial pain syndrome- a condition in which the same muscles constantly spasm.
- Muscle injury.After an injury, the pain begins to bother, and after a while they pass on their own.
- otolithiasisA condition in which calcium salt crystals accumulate in the inner ear. They cause dizziness; they are sometimes mistaken for a manifestation of diseases of the spine.
- Headache.They are also often related to degenerative changes in the cervical spine. In fact, they often have other causes.
Take care of yourself, sign up for a consultation now, without delaying treatment.
Treatment of osteochondrosis of the spine.
The standard set of therapeutic measures for exacerbation of the disease looks like this:
- Anti-inflammatories and analgesics.The doctor may prescribe Voltaren, Movalis, ibuprofen and other medications.
- If the pain is very strong and does not go away- use novocaine lock. The doctor, armed with a needle and syringe, injects an anesthetic into special places where it blocks the transmission of pain nerve impulses.
- Physiotherapy helps:drug electrophoresis with novocaine, ultrasound, ultraviolet radiation, diadynamic currents.
- If the pain constantly puts you in nervous tension,Prescribe medications to help you calm down.
- to the area of painapply dry heat.
- To download the column,Different types of traction are used. The patient can be placed on a special bed with a raised headboard and fixed with rings under the armpits. Underwater traction is also used in the pool.
- The doctor may recommendvisits to a chiropractor, acupuncture sessions.
- During an exacerbationuse special orthopedic devices that help unload the muscles and support the spine - corsets, Shants collar.
When the exacerbation passes, you need to take measures that will help prevent a new one. Therapeutic exercises and massages help strengthen the muscles that support the spine. Appoint physiotherapy courses. Good for swimming. All methods of treatment for osteochondrosis have contraindications, they must be used with caution, therefore self-medication is not the best option. Visit a doctor.
Sometimes the symptoms of the disease, despite treatment, continue to grow, the patient's condition worsens. In this case, the neurologist may raise the question of surgical treatment.

Why should you visit a doctor soon? First of all, "real" osteochondrosis is not such a harmless disease. Over time, it can make a person disabled if left untreated. Second, the symptoms can be caused by the myofascial pain syndrome itself: a neurologist will be able to quickly detect the cause of the pain and eliminate it.
Back pain is a symptom that, according to statistics, more than 90% of people have experienced at least once in their lives. Most often it is attributed to osteochondrosis. Not everyone who experiences back pain goes to the doctor. Many treat themselves with drugs that can be obtained without a prescription at a pharmacy, folk remedies. Sometimes such "treatment" gives temporary relief, and in the meantime the disease can continue to progress, and perhaps the next time the back or lower back "sprains" much more.
An experienced neurologist will be able to correctly assess the symptoms of osteochondrosis, understand its causes and prescribe the correct treatment for osteochondrosis.
With pain - the main manifestation of osteochondrosis - you can fight more or less successfully for a long time with the help of painkillers and anti-inflammatory drugs, some folk remedies. But this does not solve the main problem, the pathological changes in the spine continue to grow.
Over time, this is fraught with compression of the spinal cord and the arteries that feed it, the development of serious neurological complications: severe weakening, up to complete loss, of movement and sensitivity, poor control of the bladder, rectum.
Stages of development of cervical osteochondrosis.
In its development, cervical osteochondrosis, as a disease, passes through several stages:
I stage. The initial period is characterized by local pain in the neck, which is aggravated by turning and tilting the head. There is a softness of the cervical lordosis and muscle tension. Morphological changes in the structure of the intervertebral discs begin: drying of the nucleus pulposus, cracks in the fibrous ring.
II stage. Neck pain increases with irradiation to the arm, shoulder. Strong headaches, weakness, decreased efficiency join. The destruction of the fibrous ring continues, signs of pathological mobility and instability of the vertebrae appear.
Stage III. The pain in the neck is strong, constant, radiating to the arms and shoulders. The muscles of the hands weaken, numbness of the upper extremities is noted. Patients have headaches, dizziness, disturbances of orientation in space. At this stage, the annulus fibrosus is completely destroyed. The gelatinous nucleus pulposus is not fixed, it goes beyond the vertebrae and enters the spinal canal, forming a hernia. The hernia bulge compresses the nerves and blood vessels, leading to poor blood circulation in the cervical spine.
IV stage. This is the final stage of the disease. The cartilage of the intervertebral discs is replaced by connective tissue, the adjacent segments of the spinal column are involved in the pathological process. The joints grow together, become immobile (ankylosis). The patient's condition is serious: severe pain not only in the neck, but also in the arms, in the chest, between the shoulder blades, signs of stroke, sensitivity disorders. This is a life-threatening condition that can lead to a stroke.
The success of treatment depends 90% on the experience and qualifications of the doctor.
Diagnostics
Diagnosis of osteochondrosis of the cervical spine is made on the basis of: patient complaints, a characteristic clinical picture, an anamnesis of the disease, data from a neurological and orthopedic examination of the patient using modern diagnostic methods: radiography, magnetic tomography and computerizedand the results of the functional tests.
After making an accurate diagnosis, the doctor decides how to treat osteochondrosis of the neck in this patient, which technique should be applied in a particular case.
Treatment of osteochondrosis of the cervical spine.
Cervical osteochondrosis is treated symptomatically, mainly by conservative methods, which include:
- Pharmacological therapy, including pain relievers, anti-inflammatories, muscle relaxants, B vitamins.
- Physiotherapy methods: electrophoresis, laser therapy.
- Manual therapy.
- Acupuncture.
- Physiotherapy.
Surgical intervention is used very rarely when there is a real threat of developing a stroke, paralysis or violation of internal organs.
At this stage of the development of medical science, osteochondrosis of the cervical spine cannot be completely cured, but further progress of the pathological process can be prevented, and the state of the affected spinal segment can be stabilized.
An integrated approach, the conservative nature of the applied therapeutic methods allows you to effectively treat even advanced forms of cervical osteochondrosis.
The main methods of treatment of cervical osteochondrosis in a modern clinic.
Manual therapy and osteopathy. This method of manual impact on problem areas of the spine, the purpose of which is to restore the normal physiological position of the vertebrae and intervertebral discs. During the procedure, the pinching of the nerve roots of the spine is removed, the muscles of the neck are relaxed in the area of pathological changes.
Electrophoresis is a method of administering drugs directly to the area of the affected spinal segment. Prescribe drugs that improve blood circulation, relieve inflammation and muscle spasm.
Photodynamic phototherapy. The method is based on the ability of a photosensitive preparation to be activated by laser radiation. A layer of a medicinal substance is applied to the skin in the area of the affected segment, which, penetrating deep into the tissues by 10-13 cm, has an anti-inflammatory and analgesic effect.
The author's three-component technique, including manual therapy, electrophoresis and laser therapy, allows you to quickly relieve pain, remove swelling from surrounding tissues, improve blood supply to the area of inflammation and activate metabolic processes of damaged cartilage tissue. intervertebral discs. The goal of treatment is not only to reduce pain and improve the patient's condition, but also to act on various parts of the pathological process in order to stop further destruction of the intervertebral discs and the destruction of the vertebrae themselves.
The techniques used for the treatment of osteochondrosis of the neck in modern clinics have been tested in the best manual therapy centers in Europe and the USA, they are safe, effective, have practically no contraindications and are well tolerated even by elderly patients. age. groups
Recommendations on what to do with cervical osteochondrosis, the patient will receive after consulting a neurologist, depending on the stage of the disease, the severity of symptoms, comorbidities and the results of the examination.
Osteochondrosis of the cervical region
Osteochondrosis of the neck is a degenerative disease in which literally "premature aging" occurs, "wearing out" of the intervertebral discs, joints, vertebrae of the cervical spine.
Some facts about the disease:
- Osteochondrosis of the neck occurs in men and women with the same frequency.
- Most often, people from 30 to 60 years old get sick.
- As a rule, pathology occurs in people who at work have to constantly be in the same position and perform monotonous movements.
- The cervical spine has some structural features, so the disease can have many different manifestations.

What features of the cervical spine cause the symptoms of osteochondrosis?
- There are openings in the lateral processes of the vertebrae - carotid arteries pass through them on the right and left, which supply blood to the brain.
- In the cervical region passes the initial part of the spinal cord: it contains fibers that carry nerve impulses to all parts of the body, provide movement, sensitivity. If there is compression of the spinal cord in the neck, neurological disorders occur throughout the body.
- This section of the spine is highly mobile, and this predisposes to the onset of osteochondrosis (although, in most cases, the disease still develops in the lumbar region - not only is it highly mobile, but it also experiences the increased stress).
- In the neck, nerve roots emerge from the intervertebral foramina, forming the cervical and brachial nerve plexuses. They are responsible for movements in the muscles of the neck, arms, shoulder girdle, skin sensitivity, regulation of autonomic functions.
- The first vertebra does not have a massive front part, the body, it is a bone ring that is placed on the tooth, a bone growth on the second vertebra. This allows the head to turn from side to side.
Neck pain, headaches, a feeling of weakness, numbness in the hands are symptoms that should see a neurologist. Examination by a specialist and examination using modern equipment will help to understand the causes of the pathology and take the most effective measures.
What happens to the vertebrae in cervical osteochondrosis?
The incomprehensible medical term "degenerative process" refers to the following pathological changes that occur in the cervical spine:
- First of all, the lesion in osteochondrosis covers the intervertebral discs. They become thinner, thereby reducing the distance between adjacent vertebrae. Small holes, microcracks, are formed on its outer part. Over time, this can lead to a herniated disc.
- As a result of damage to the discs, the stability of the connection of the vertebrae is disturbed.
- Suffers with osteochondrosis of the cervical and intervertebral joints - spondyloarthrosis develops. It also promotes compression of the nerve roots.
- The pathological process extends to the vertebrae themselves. Due to the fact that the functions of the intervertebral discs are impaired, the load on them increases. The spine tries to compensate for this violation, bone growths appear - osteophytes.
Treatment of osteochondrosis of the cervical spine.
During an exacerbation of osteochondrosis of the cervical vertebra, traction is used (the patient is placed on a bed with a raised head, and the head is fixed with a special tie) to unload the intervertebral discs. For the same purpose, you need to wear a Shants necklace. To relieve pain, analgesics and anti-inflammatories are prescribed. With severe pain that does not go away, the doctor can perform a blockade - inject an anesthetic solution into the area of the affected nerve roots. Physiotherapy is used: ultrasound treatment, novocaine electrophoresis.
When the exacerbation subsides, the treatment of osteochondrosis of the cervical spine includes massage, physical therapy, physiotherapy.
One of the main signs of cervical osteochondrosis is pain in the neck. Many people who are faced with this symptom do not go to the doctor, preferring to treat "chondrosis" with home methods. There are at least two good reasons to refuse self-treatment and consult a specialist doctor.
First of all, painkillers and folk methods, although they help relieve pain for a while, do not solve the main problem. Pathological changes in the spine continue to grow. Over time, this threatens with more serious consequences. To the extent that surgery is required.
Secondly, neck pain occurs not only with osteochondrosis. There are many other reasons. Only a doctor can understand and prescribe the proper treatment.
Physiotherapy
Treatment of lumbar osteochondrosis is a long process.that require an integrated approach. After getting rid of the primary symptoms, you can proceed to the use of various physiotherapy procedures:
- UHF therapy.Exposure to high frequency electromagnetic fields. It has an anti-inflammatory, analgesic effect, and also promotes the start of regenerative processes.
- Amplipulse.Low-frequency currents are applied to problem areas of the body. There is an expansion of blood vessels, eliminating pain and spasms.
- Phonophoresis and electrophoresis.The introduction of drugs into deep tissues using ultrasound and direct current.
Massage procedures are also widely used, which are possible only after the elimination of the inflammatory process. Massage promotes muscle relaxation, eliminating spasms.
Diet - complex treatment of osteochondrosis.
With this disease, it is necessary to act in a complex way, so changing the diet is a completely effective method of treatment. The diet is fairly consistent with the generally accepted understanding of the concept of healthy eating, so try adding the following types of foods to your diet:
- Citrus (in the absence of allergies).
- Olive oil.
- Fresh herbs and vegetables.
- Mineral water.
- Fish and foods rich in phosphorus, protein, magnesium and calcium.
- Dairy and milk products.
An excellent auxiliary tool will be ready-made vitamin complexes, which can be found in a wide variety in pharmacy chains. Remember that all medications should be taken only as prescribed by a doctor.
What symptoms of osteochondrosis of the cervical spine should make you see a doctor?
The main symptom of cervical osteochondrosis is pain. It can occur in different places, depending on the level at which the pathological process is localized: in the neck, in the shoulder girdle, in the arm, in the region of the heart. By nature, pain sensations are deaf, they can be burning, aching.
Other manifestations of the disease:
- Headaches, dizziness, "flies before the eyes", noises, ringing in the ears.
- Weakness in the muscles of the neck, shoulder girdle, arms.
- Violation of skin sensitivity.
- Shoulder-shoulder periarthritis: painful pain in the neck that passes to the arm, difficulty in abducting the arm above 90°, weakness and atrophy of the muscles of the shoulder girdle.
- Shoulder-hand syndrome: pain in the shoulder and hand, swelling and stiffness of the fingers, weakness and atrophy of the hand muscles.
- Vertebral artery syndrome. Bone growths appear on the vertebrae, which compress the nerves, causing a reflex spasm of the vertebral artery, which is involved in the blood supply to the brain. The symptoms of cervical osteochondrosis are joined by constant headaches that start from the back of the head, spread to the temple, to the crown, nausea, noises in the head, ringing in the ears, flashing of bright spots before the eyes.
- Anterior scalene syndrome. There is an anterior and middle scalene muscle in the neck - they are close, and between them there is a small gap in which nerves and blood vessels pass. With osteochondrosis of the cervical spine, the anterior scalene muscle tightens and squeezes them, which causes symptoms such as pain on the inner surface of the forearm, shoulder and fingers. Sometimes the pain radiates to the back of the head. The skin on the hand may become cold, pale, and numbness occurs.
- epicondylitis syndrome. At the bottom of the shoulder, on the sides of the elbow joint, there are bony protrusions - epicondyles. With epicondylitis syndrome caused by cervical osteochondrosis, pain occurs in them, which increases when pressed. Other symptoms also occur: pain in the neck, pain when pressing certain points in the region of the cervical vertebrae.
If two sections of the spine are affected at once, with cervicothoracic osteochondrosis, symptoms may include pain between the shoulder blades, in the region of the heart.
With osteochondrosis, the risk of intervertebral hernia and stroke increases. If you experience any of the symptoms listed above, see your doctor.
conclusion
Now you know how to treat osteochondrosis of the cervical spine without resorting to the use of surgical intervention. The operation is the most radical method of treatment when the disease is already running and there is no other way out. But it is in your power to do so so as not to bring your health to such a state.






























